Restricted blood circulation speeds tumor progress by getting old the immune system. The findings spotlight dangers for sufferers with vascular illness and potential new therapies.
A brand new research from NYU Langone Well being stories that restricted blood circulation can speed up the getting old of bone marrow, lowering the immune system’s means to fight most cancers.
The analysis, printed on August 19 in JACC-CardioOncology, discovered that peripheral ischemia—restricted circulation within the arteries of the legs—brought on breast tumors in mice to develop at twice the speed noticed in mice with regular blood circulation. These outcomes construct on a 2020 investigation by the identical workforce, which confirmed that ischemia throughout a coronary heart assault produced comparable results.
How ischemia develops
Ischemia develops when fatty substances, akin to ldl cholesterol, construct up inside artery partitions. This buildup triggers irritation and clot formation, which restrict the supply of oxygen-rich blood. When ischemia happens within the legs, it ends in peripheral artery illness, a situation that impacts thousands and thousands of Individuals and raises the probability of coronary heart assault or stroke.
“Our research reveals that impaired blood circulation drives most cancers progress no matter the place it occurs within the physique,” says corresponding writer Kathryn J. Moore, PhD, the Jean and David Blechman Professor of Cardiology within the Division of Drugs, Leon H. Charney Division of Cardiology, NYU Grossman Faculty of Drugs. “This hyperlink between peripheral artery illness and breast most cancers progress underscores the important significance of addressing metabolic and vascular threat elements as a part of a complete most cancers remedy technique.”
The investigators additionally found that restricted circulation shifts the stability of immune cell populations in a method that weakens the physique’s means to battle infections and most cancers. These alterations intently resemble the adjustments in immune operate that usually happen with getting old.
Systemic skewing of immune cells
To analyze how cardiovascular disease influences cancer progression, the researchers created a mouse model carrying breast tumors and induced temporary ischemia in one hind limb. They then compared tumor development between animals with restricted circulation and those with normal blood flow.
The results expand on what is known about the immune system, which has evolved to defend against invading bacteria and viruses and, under healthy conditions, to recognize and destroy cancer cells. These defense mechanisms depend on stem cell reserves in the bone marrow that can be activated when needed to generate crucial white blood cell populations throughout life.
Under typical circumstances, the immune system counters infection or injury by increasing inflammation to eliminate harmful agents and later scaling it back to protect healthy tissue. This balance relies on a mixture of immune cells that either amplify or suppress inflammation. The investigators discovered that limited blood flow disrupts this equilibrium by reprogramming bone marrow stem cells. The shift favors the production of “myeloid” immune cells (monocytes, macrophages, neutrophils), which weaken immune defenses, while decreasing the generation of lymphocytes such as T cells that are vital for mounting strong anti-cancer responses.
Tumor environment shifts toward suppression
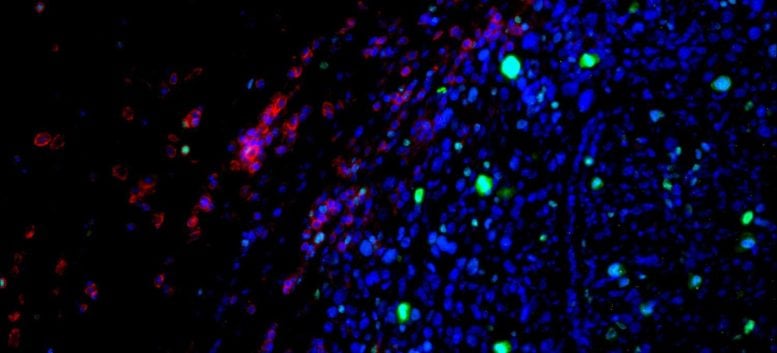
The local environment within tumors showed a similar shift, accumulating more immune-suppressive cells– including Ly6Chi monocytes, M2-like F4/80+ MHCIIlo macrophages, and regulatory T cells – that shield cancer from immune attack.
Further experiments showed that these immune changes were long-lasting. Ischemia not only altered the expression of hundreds of genes, shifting immune cells into a more cancer-tolerant state, but also reorganized the structure of chromatin–the protein scaffolding that controls access to DNA–making it harder for immune cells to activate genes involved in fighting cancer.
“Our results reveal a direct mechanism by which ischemia drives cancer growth, reprogramming stem cells in ways that resemble aging and promote immune tolerance,” says first author Alexandra Newman, PhD, a postdoctoral scholar in Dr. Moore’s lab. “These findings open the door to new strategies in cancer prevention and treatment, like earlier cancer screening for patients with peripheral artery disease and using inflammation-modulating therapies to counter these effects.”
Moving forward, the research team hopes to help design clinical studies that evaluate whether existing inflammation-targeted therapies can counter post-ischemic changes driving tumor growth.
Reference: “Cancer Development in Atherosclerotic Cardiovascular Disease: JACC: CardioOncology Short-Form Primer” by Jessie M. Dalman, BA and Kathryn J. Moore, 19 August 2025, Cardio Oncology.
DOI: 10.1016/j.jaccao.2025.05.016
The study was supported by American Heart Association grants 915560, 25CDA1437452, 23POST1029885, 25PRE1373174, and 23SCEFIA1153739; as well as by National Institutes of Health grants T32GM136542, F30HL167568, T32HL098129; R01 HL151078, R01 HL161185, R35 HL161185, R01HL153712, R01HL172335, R01HL172365, and P01HL131481. The work was also supported by the Sarnoff Cardiovascular Research Foundation, the LeDucq Foundation Network, and Laura and Isaac Perlmutter Cancer Center support grant P30CA016087.
Never miss a breakthrough: Join the SciTechDaily newsletter.